Description and principle of operation of the lamp from jaundice
What is a jaundice lamp
In 32-86% of newborns in the first week of life, mainly on the second or third day, the so-called physiological jaundice is noted, which is manifested externally by yellowness of the skin and sclera of the eyes.
The phenomenon itself is not abnormal and occurs due to a reduced level of liver enzymes and, as a result, an insufficient rate of breakdown in the liver of indirect bilirubin, formed during the decomposition of dying red blood cells and hemoglobin. The most common reason is:
- prematurity and / or low weight of the child;
- endocrine disorders in the mother, especially diabetes mellitus and thyroid disease;
- Rh-conflict of the blood of mother and child;
- gestosis during pregnancy.
For the full development of the enzyme system of the child, it takes from one and a half to three months. In the initial period of formation, therapy is aimed at combating hyperbilirubinemia. It is indirect bilirubin that poses the greatest danger to the newborn due to its histotoxicity - the ability to adversely affect metabolic processes in tissues, including the brain.
There are 25 known forms of neonatal jaundice, and only the rarest of them require medical or surgical treatment. In 95% of cases, this condition is compensated by phototherapy with lamps emitting a spectrum of light close to ultraviolet.
How it works
Under the influence of lamps emitting light with a wavelength of 400-500 nm, photoisomerization of indirect bilirubin molecules occurs in the skin with its transition to a water-soluble form. The resulting direct bilirubin is not dangerous and is easily excreted by the excretory systems of the body in urine, feces and, to some extent, sweat.

The therapeutic effect is manifested:
- laboratory - a decrease in the level of bilirubin in the blood already on the second day of phototherapy and complete normalization on days 5-6;
- visually - a decrease in the yellowness of the skin, mucous membranes and sclera of the eyes on the third or fourth day of treatment.
Note. Dark green coloring of neonatal stools during phototherapy is normal due to the excretion of direct bilirubin and is not dangerous. It can be taken into account as an additional indicator of the effectiveness of lamp treatment.
It was experimentally determined that the highest degree of photoisomerization is achieved when irradiated with blue spectrum light and a narrow wavelength of 450–460 nm. Application ultraviolet lamps not so effective for newborns, since their operating range lies in the range from 100 to 400 nanometers, which is dangerous for the fragile body of babies.
Varieties
Depending on the design, there are lamps:
- upper light - mounted on a portable stand or in a stationary panel connected to the hood. The main disadvantage is the requirements for the protection of the genitals and organs of vision in the case of the use of light sources close to the aggressive ultraviolet range;

- lower light - lamps located at the bottom of a case with a transparent bottom, or under a hammock with a translucent fabric. Less demanding on eye protection, provided that the child’s posture is observed or safe LED lamps are used;

- wrapping - a fabric with a fiber optic cable located on the inner surface of a blanket or bedspread. The development of American scientists is considered safe and convenient, since the rays of light are directed inward and do not fall into the eyes, and the small volume of the folded blanket allows you to carry it with you and use it wherever there is a power source.

As an alternative to lamps in countries with a warm climate, sunlight is used, passed through a special filter cloth. This material cuts off the ultraviolet and infrared range, passing only the blue spectrum of visible light.The child is placed under a canopy made of filter cloth, and is under it undressed throughout the day. Studies have shown that the therapeutic effect of filtered sunlight is not inferior, and in some groups even exceeds that of phototherapy with electric lamps. The only drawback of the method is the need to monitor the temperature of the baby, and when the body is heated to 38 ° C, place it in the shade until the thermometer returns to normal.
Structural differences between photolamps and jaundice for the comfort of the newborn and the result of treatment are not of fundamental importance, since different types of lighting elements can be used in the same installations. Some types of lamps have a limited useful life. This means that the efficiency of an externally working device decreases over time. New devices are equipped with special meters that mark the "mileage" of the lamp. The condition and efficiency of a lamp without a counter is determined by a photometer.
Newborn jaundice: causes, treatment
LED or LED devices
The most economical and safe light sources. It is the LEDs that are mounted in cuveuses with a transparent bottom. Since these lamps practically do not heat up, they can be placed at any convenient distance from the baby’s body, and the intensity of the blue spectrum with a wavelength of 420-470 nm with a power of 500 μW / cm2 at a distance of 800 mm from the body eliminates the harmful effects of high- and low-wave radiation. The peculiarity of LED-devices is that their light is less effective, but at the same time relatively safe for the organs of vision and skin of the newborn. Another positive difference between LEDs is their resource, which is 20,000-50,000 hours of operation.LED lamps are a complete replacement for halogen and fluorescent devices.

Halogen lamps
Improved incandescent lamps with a tungsten filament located in a bulb with iodine or bromine vapor. Light filters are used to cut off unnecessary radiation waves, however, halogen lamps operate in the range of 380-600 nm, and their light output reaches 22 Lm / W, which places special demands on the protection of the organs of vision and inguinal region from light burns. In addition, the flask heating temperature of 300 °C implies the placement of the device at a distance from the patient in order to avoid hyperthermia, which reduces the concentration of the light flux. The duration of the halogen devices is a maximum of 4000 hours. The uneven distribution of the useful spectrum and increased requirements for the control of possible hyperthermia and overdose of UV radiation make the use of halogen lamps in devices for the treatment of hyperbilirubinemia impractical.

Fluorescent photo lamps
Most often used as bactericidal, since the electrical discharge in mercury vapor is capable of producing a wide range of light waves, starting from the green visible spectrum with a length of 520 nm up to aggressive low-wave ultraviolet class B. For the treatment of jaundice, gas discharge devices with turquoise - 490 nm and blue light - 420-460 nm are suitable . In terms of energy consumption, they are not inferior to LEDs with the same light output, and the working life reaches 70 thousand hours. Low heat transfer does not lead to hyperthermia and allows the installation of fluorescent flasks in devices without special radiators and forced cooling. Some disadvantages:
- the presence of toxic mercury inside a fragile flask;
- frequent breakdowns of starting devices;
- burnout of light-forming photocells and photofilters in the flask with a change in the operating range to the ultraviolet side.
All this requires attention to the conditions of use, maintenance and protection of the eyes and groin of the child from burns. In this, fluorescent lamps are inferior to LED.

hybrid
Combination of upper and lower light lamps, when LED lamps are installed in the bottom of the cuveaux, and halogen or fluorescent lamps. In some cases, combinations of low light with a photo-optic cover are used. Combined systems are used when it is necessary to achieve the maximum effect in a short time, but the application requires special skills from the attendants.

How to choose the right lamp
The stationary conditions of neonatal centers allow the use of any types of devices and their combinations, since professional doctors monitor all the indicators and the condition of the baby. In cases where the attending physician allows phototherapy at home, the conditions for choosing a device for the treatment of neonatal jaundice are:
- Safety.
- Mobility.
- Ease of use.
Two types of lamps fit these criteria:
- portable incubators with lower light or tripods on LED-elements. They do not harm the organs of vision, practically do not lead to an overdose of UV, hyperthermia. As a rule, they are equipped with an electronic control system with a programmable operating mode and a counter showing the remaining useful life. At the same time, they are relatively affordable and economical;
- photo blankets and photo covers.They have all the advantages of LED lamps, but at the same time they do not cause anxiety for a newborn, when folded they are placed in a small case. The main and only drawback is the high price and a small assortment on the medical equipment market.
Under the condition of a short course of treatment, it is not advisable to purchase such equipment, so most parents are limited to the services of companies that provide the device for rent.

Indications and contraindications for use
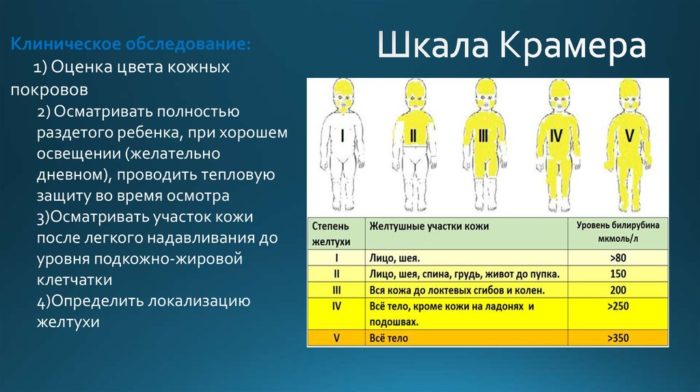
The final decision on the advisability of using a conservative method of treating neonatal jaundice is made by a neonatologist or a local pediatrician. The appointment of phototherapy is possible on the basis of examination data, laboratory tests and maternal history, including during pregnancy. Most often, light therapy is indicated in the following cases:
- physiological jaundice of newborns with the level of indirect bilirubin in full-term ones is above 70 µmol/l, in premature babies 60 µmol/l.
- mild hemolytic disease of the newborn, when the level of indirect bilirubin in the blood serum does not exceed 60 μmol / l;
- the presence in the anamnesis of the mother of diabetes mellitus, thyroid pathologies, severe gestosis, anemia during pregnancy;
- physiological immaturity of a premature newborn;
- preparation or rehabilitation before / after surgical interventions;
- the presence of subcutaneous and parenchymal hemorrhages in a child.
Absolute contraindications for phototherapy include:
- cholestasis due to obstruction of the bile ducts;
- "bronze baby" syndrome - increased photosensitivity of the skin, when phototherapy leads to a grayish-brown staining of the skin, urine and discoloration of the feces;
- inflammatory processes in the liver tissues;
- a critical level of bilirubin, which poses a danger to the life of a child due to damage to the central nervous system:
- for full-term 342 µmol/l;
- for premature babies 270 µmol/l;
- for deeply premature babies from 170 µmol/l.
In the presence of contraindications and in cases of ineffectiveness of phototherapy, when there is no time for conservative therapy, drug treatment is used, and in some cases surgery is indicated.
Instructions for use
Fluorescent lamps
- Clothes are removed from the newborn, leaving the diaper, special goggles are put on with fixation under the chin to prevent involuntary slipping and placed in an incubator.
- The device is turned on and installed at a distance of 400-600 mm from the child's body.
- A timer is set for 30 minutes. up to 8 hours, depending on the instructions of the neonatologist.
- The session is interrupted for feeding, diaper change. If redness of the skin is detected and the child is very anxious, the doctor should be notified.

Halogen lamps
Due to the wide spectrum of radiation with the capture of the ultraviolet range and the heating of the bulb up to 300 ° C, halogen lamps are used with the most careful approach to safety, including:
- mandatory use of eye protection and genital area;
- placing the lamp no closer than 800 mm from the child;
- control over body temperature and detection of hyperemic skin areas.
For treatment with halogen devices, it is recommended that the child be in a hospital.
Combined systems
In the case of using combinations of luminescent and LED light sources, the tactics of treatment correspond to the standard for a particular type of device.If the combined system means therapy with a photoblanket with a fiber optic surface, then the method of its use implies:
- exclusion of protective devices;
- daily cycle of therapy with breaks for hygiene procedures;
- the possibility of feeding without taking the newborn out of the photosuit or blanket.

LED lamps
- The child is undressed completely or to the diaper. A cap or goggles is placed over the eyes to improve the quality of sleep.
- The patient is placed under the apparatus, in an incubator or a hammock, face up.
- Using the control panel, the operating mode and session time specified by the attending pediatrician are set.
Duration of treatment
It is forbidden to independently determine the necessary course of treatment and the duration of periods of phototherapy. With home treatment, the district pediatrician is obliged to examine the patient and monitor the course of therapy throughout the course. Parents or nannies follow all the doctor's instructions. In the normal course of phototherapy, the yellowness of the skin completely disappears on the 7-8th day. The manifestation of symptoms on the first day or persistent jaundice for more than 14 days is an abnormality and a reason to transfer the patient to a hospital for additional examination and outpatient treatment.
Adverse reactions when using lamps
Prolonged exposure to the blue spectrum of light, even with full observance of safety precautions, is sometimes accompanied by:
- hyperemia of the skin, sometimes burns;
- dryness and peeling of the epidermis;
- hyperthermia;
- stool disorder;
- increased anxiety, sleep disturbance.
In order to prevent violations of the water balance, the child is given water or 0.9% NaCl from a spoon, and in severe cases, infusion therapy is performed with a 3% glucose solution.
How quickly does bilirubin decrease?

The final formation of the enzymatic system of the liver of a newborn occurs by 1.5-3.5 months of life. Throughout the period, complications and relapses are possible. Treatment is considered effective if the decrease in the level of indirect bilirubin in the patient's blood occurs by 19-21 μmol / day.